Retinal Tears and Detachments
Retinal Tears
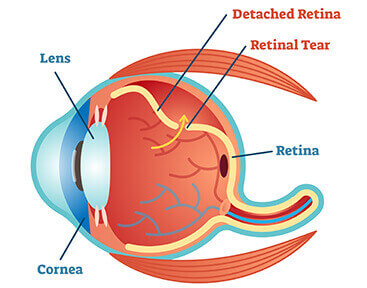
The retina is the light-sensitive tissue that lines the inside of the back of the eye. This layer of tissue helps to generate vision by its connection to the brain through the optic nerve. The eye is composed of a gel (vitreous) which liquifies over time. The vitreous is attached to the retina but can separate (posterior vitreous detachment) and pull on the retina leading to a painless tear in this sensitive tissue. If fluid from inside the eye goes into this defect in the retina, the fluid will lift the retina off the back wall of the eye causing a retinal detachment.
Causes:
- Normal age-related changes
- Myopia (Near-sightedness)
- Lattice Degeneration (thin areas of retinal tissue)
- Trauma
- Family or Personal History
- Prior eye surgery (i.e.- cataract surgery)
Symptoms:
There is no way to predict who will develop a retinal tear or when it will occur. Patients should look out for the following signs and symptoms.
- Flashes of light (usually off to the side) lasting for just a few seconds
- Floaters (increase in the size or number of floaters) in your vision
- Curtain or veil in your central or side vision
If you notice any of these symptoms you should contact us immediately, at (800) 255-7188.

Diagnosis and Treatment:
A thorough dilated eye exam with the aid of firm but gentle pressure on the eye (scleral depression) will be performed by your surgeon to help with the diagnosis and treatment of retinal tears. If diagnosed early, before fluid gets underneath the retina, an in-office procedure can often be used to spot-weld (create strong adhesions with a scar) around the tear. Timely treatment can prevent a retinal detachment and vision loss.
- Laser retinopexy
- Cryotherapy (freezing)
Continued follow up with your retinal surgeon is recommended to assure good adhesion of the treatment and to diagnose subsequent retinal tears that may develop. At Central Florida Retina our physicians have been diagnosing and treating retinal tears for over 40 years. For further information or to book an appointment call 800-255-7188.
Retinal Detachment
The retina is the light-sensitive tissue that lines the inside of the back of the eye. This layer of tissue helps to generate vision by its connection to the brain through the optic nerve. If a retinal tear or hole is present in this tissue layer and fluid from inside the eye goes into these defects the fluid will lift the retina off the back wall of the eye causing a retinal detachment. Initially the fluid will be localized but over time the fluid will spread and can lead to permanent vision loss. The lifetime risk in normal eyes is around 1:300 and can be as high as 1:20 in patients with high myopia (>6 diopters). Although retinal detachment usually occurs in one eye, there is around a 15% chance of developing it in the other eye.
Symptoms:
There is no way to predict who will develop a retinal detachment or when it will occur. Patients should look out for the following signs and symptoms.
- Flashes of light (usually off to the side) lasting for just a few seconds at a time
- Floaters (increase in the size or number of floaters) in your vision; floaters can appears as small, dark, shadowy shapes that can look like spots, thread-like strands, or squiggly lines in your vision
- Curtain or veil in your side vision that progresses towards your center of vision
- Blurred Vision
- Curved or wavy lines (metamorphopsia)
If you notice any of these symptoms you should contact us immediately, at (800) 255-7188.
Types of Detachment:
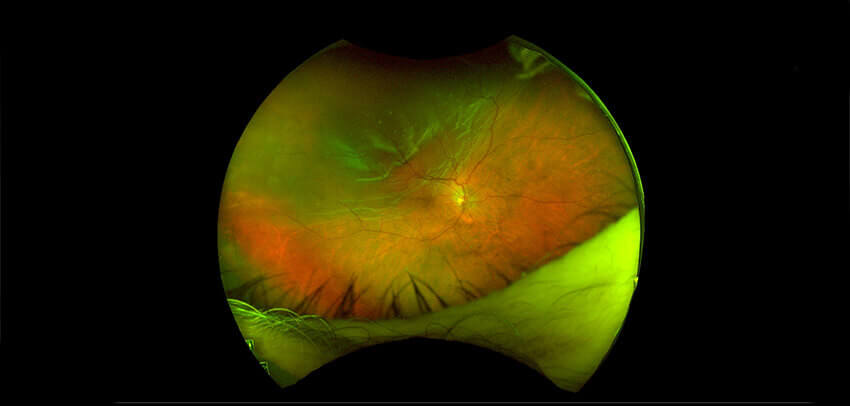
Rhegmatogenous retinal detachment
A rhegmatogenous retinal detachment occurs due to a hole, tear, or break in the retina that allows fluid to pass into the subretinal space between the sensory retina and the retinal pigment epithelium. Most occur spontaneously due to a tear in the retina, which can occur during vitreous separation.
The most common causes include, but not limited to the following:
- Normal age related changes
- Myopia (near-sightedness)
- Lattice degeneration (thin areas of retinal tissue)
- Trauma
- Family or personal history
- Prior eye surgery (ie- cataract surgery)
Exudative or secondary retinal detachment
An exudative retinal detachment occurs due to inflammation or injury that results in fluid accumulating underneath the retina without the presence of a hole, tear or break.
The most common causes include, but not limited to the following:
- Wet macular degeneration
- Central serous chorioretinopathy
- Vogt-Koyanagi-Harada syndrome
- Choroidal tumors (melanoma, metastasis, etc)
- Other uveitic (inflammatory) processes
Tractional retinal detachment
A tractional retinal detachment occurs when fibrovascular (scar) tissue that has developed on the surface of the retina caused by an injury, inflammation or diabetes pulls the sensory retina from the underlying layer of the tissue.
The most common causes include, but not limited to the following:
- Diabetic Retinopathy
- Sickle Cell Retinopathy
- Other processes leading to the formation of abnormal vessels in the eye
Diagnosis and Treatment:
A thorough dilated eye exam with the aid of firm but gentle pressure on the eye will be performed by your retinal surgeon to help with the diagnosis and planning of treatment for your retinal detachment. Timely treatment may prevent loss of vision. The goal of the surgery is to reattach the retina to the wall of the eye. There are several options for treating a detached retina. You and your surgeon will discuss the best personalized options for the treatment of your retinal detachment.
Laser Barricade:
In certain cases if the retinal detachment is caught early enough thermal burns can be used to surround the fluid and prevent the spread of the retinal detachment. This can usually be done in the office.
Pneumatic Retinopexy:
In office procedure using a gas bubble and either cryotherapy or laser to help reattach the retina. The gas bubble helps to temporarily seal the retinal breaks/holes while your body removes the fluid from underneath the retina. The laser or cryotherapy will help to form a permanent scar to keep the retina attached. Your surgeon will ask you to position in a specific way to cover the holes/tears.
Pars Plana Vitrectomy:
A microsurgical procedure used to remove the vitreous gel (floaters) with three small incisions in the white part of the eye (sclera). This is done in an operating room under a microscope. A large gas or silicone oil bubble will be placed in the eye to seal the retinal tears/holes while the laser or cryotherapy forms a permanent scar/adhesion around these defects. Your surgeon will ask you to position in a specific way to cover the holes/tears.
Scleral Buckle:
A small silicone band or sponge is placed around the eye. This band helps to support the eye from the outside by pushing the eye wall inwards to help close the holes/tears. The band does not normally have to be removed. Often these will elongate the eye and lead to further increase in myopia (nearsightedness). Your surgeon may ask you to position in a specific way to cover the holes/tears if a gas bubble is placed in the eye.
In general, retinal detachment repairs succeed in about 9 out of 10 cases in one surgery, though more than one procedure can be required to successfully put the retina back into place. Continued follow up with your surgeon is recommended to assure good adhesion of the retina over time. At Central Florida Retina our physicians have been diagnosing and treating retinal detachments for over 40 years. For further information or to book an appointment call 800-255-7188.



